Cardiac Electrophysiology is a rapidly growing subspecialty of cardiology which focuses on the diagnosis and treatment of cardiac arrhythmias. The cardiac electrophysiology (or “EP”) laboratory is a specialized invasive procedure area where various procedures are performed, including diagnostic electrophysiology studies, catheter ablations, pacemaker and implantable cardiac defibrillator (ICD) implantations, Laser extraction of pacemaker and ICD leads, and implantation of biventricular pacing devices for treatment of congestive heart failure.
Good Samaritan Hospital is on the forefront of innovative techniques to treat complex cardiac arrhythmias utilizing implantable devises. Good Samaritan Hospital is the only hospital in
Rockland and Orange counties to offer the Left
Atrial Appendage Closures (LAAC) utilizing the WATCHMAN devise procedure.
Request an Appointment or Refer a Patient | Call 845.533.7125 or 845.368.5953.
Cardiac Electrophysiology (EP) Studies at Good Samaritan Hospital
The heart has an electrical system which controls its rhythm. The normal “pacemaker” of the heart is the sinus node in the top of the right atrium; one of the upper chambers of the heart, which normally initiates and controls the heart rate. The electrical activity then travels to the AV node in the middle of the heart which holds and delays the activity to allow time for the top chambers to pump the blood to the bottom chambers. It then travels to and stimulates the bottom 2 chambers (“ventricles”) which then pump the blood to the body and to the lungs.
Abnormalities in the heart's electrical system can cause slow rhythms such as sinus bradycardia or heart block, fast heart rhythms such as atrial fibrillation or flutter, supraventricular tachycardia, ventricular tachycardia, or ventricular fibrillation. These abnormal rhythms can cause symptoms of palpitations (abnormal fluttering), lightheaded or dizzy spells, syncope (passing out) or even death.
An electrophysiology study is a safe and relatively painless test which is used to: determine the cause of symptoms; determine if a patient is at risk of an arrhythmia (abnormal heart rhythm); determine which type and where the arrhythmia originates; determine the best type of treatment (e.g. possible pacemaker, defibrillator, medication, or ablation), and potentially to treat and cure the arrhythmia.
The Electrophysiology study is done by an electrophysiologist (cardiology physician specializing in arrhythmia management) using fluoroscopy (x rays) and small catheters (tubes with small pacemaker tips), placed through the vein in the groin, and then threaded to the heart. Patients are awake (but sedated) during the procedure and don’t feel the catheters being placed into the heart. The electrophysiologist uses a computer to stimulate the heart to test the electrical system and to potentially induce (start) the abnormal rhythm. This information allows the physician to determine the best treatment. If the treatment is catheter ablation this is often done at the same time to potentially cure the abnormal rhythm. If the treatment is to be a pacemaker or implantable defibrillator (ICD) this is generally done separately, often during the same hospitalization. Medications can be used to stimulate the heart and to test the rhythm. The EP study generally takes one to two hours.
After the procedure, the catheters are removed, pressure is held, patients can remain in bed and are welcome to have their families and loved ones sit with them in the ambulatory unit. Patients are generally discharged the same day--or the following day if a pacemaker or ICD implant is required.
Pulsed Field Ablation
Our cardiac electrophysiology team at Good Samaritan Hospital has performed its first pulsed field ablation for patients with atrial fibrillation. Instead of traditional methods of ablation that use hot (Radiofrequency) or cold (Cryo) technology to damage abnormal heart tissue which can affect the surrounding organs, pulsed field ablation utilizes pulsed electric fields to effectively treat atrial fibrillation while minimizing collateral damage to surrounding heart structures. This new technology is safer, more effective, and faster than previous procedures; it can decrease procedure time from four-five hours to less than an hour. We are the only hospital offering this procedure in Rockland, Orange, Sullivan and Westchester Counties.


Left Atrial Appendage Closure (LAAC) – WATCHMAN Device
If you have atrial fibrillation that is not caused by heart valve problems (Non-valvular atrial fibrillation), and are looking for an alternative to blood thinners, Good Samaritan Hospital offers a unique one-time procedure that may reduce your risk of stroke for a lifetime without blood thinners.
Good Samaritan Hospital is the only hospital in Rockland and Orange counties to perform Left Atrial Appendage Closures (LAAC) utilizing the WATCHMAN device. Our Electrophysiologists are national proctors and have extensive experience in cardiac device implantations, completing over 140 LAAC procedures in the last 5 years.
Are You A Candidate For A Left Atrial Appendage Closure Device?
Request an Appointment or Refer a Patient | Call 845.533.7125.
Non-Valular Atrial Fibrillation (Afib) and Stroke
Atrial fibrillation (AFib) occurs when the right and left atria in the heart no longer contract in a coordinated way causing an irregular heartbeat. AFib can decrease the  heart’s pumping capacity by as much as 15-20%. The decreased blood flow and erratic heartbeat increases the chance of blood cells bonding together to create clots that can enter the bloodstream and trigger a stroke. According to the National Stroke Association, AFib patients are five times more likely to have a stroke than someone with a regular heartbeat.
heart’s pumping capacity by as much as 15-20%. The decreased blood flow and erratic heartbeat increases the chance of blood cells bonding together to create clots that can enter the bloodstream and trigger a stroke. According to the National Stroke Association, AFib patients are five times more likely to have a stroke than someone with a regular heartbeat.
Blood thinners, also called anticoagulants, are an effective way to lower the risk of stroke in people with atrial fibrillation. But some people need an alternative to blood thinners, because they have an occupation, lifestyle or medical condition that puts them at risk for excessive bleeding.
Alternative to Blood Thinners
More than 90% of stroke-causing clots that come from the heart are formed by blood pooling in the Left Atrial Appendage (LAA), the small pouch-like sac in the top left chamber of the heart. This pouch is not needed for normal functioning of the heart.
Good Samaritan Hospital offers the Left Atrial Appendage Closure (LAAC), procedure which eliminates the need for blood thinners by utilizing the WATCHMAN device to permanently close off the LAA and keep blood clots from escaping.
How the Left Atrial Appendage Closure (LAAC) Procedure Works

During the LAAC, the WATCHMAN device is implanted into the left atrial appendage. The umbrella-balloon like device is about the size of a quarter and made from very light and compact materials commonly used in many other medical implants.

Your doctor will insert a small intravenous line in your upper leg to insert a narrow tube and guide the WATCHMAN device into your heart’s left atrial appendage (LAA). Every patient’s LAA is shaped and sized differently, so our experienced team uses advanced ultrasound technology to take measurements, choose the appropriately sized device and verify proper placement over the opening of the LAA.
The self-expanding frame of the WATCHMAN seals off the LAA and acts as a filter for blood clots to prevent a stroke. The minimally invasive procedure takes about an hour and is performed under general anesthesia. Patients commonly stay in the hospital overnight and are able to leave the following day.
After Your Left Atrial Appendage Closure Procedure
Once the device is implanted, heart tissue will begin to grow over the implant and form a natural barrier against blood clots. You will continue to take blood thinners for approximately 45 days or until your LAA is permanently closed off by the growth of the heart tissue over the device. Your cardiologist and electrophysiologist will monitor this process by taking pictures of your heart to see when you can stop taking the blood thinner.
Are You A Candidate For A Left Atrial Appendage Closure Procedure?
If you answer yes to the questions below, the left atrial appendage closure procedure and WATCHMAN device may be the right choice for you:
- Have you ever been diagnosed with atrial fibrillation not caused by a heart valve problem?
- Are you currently taking or have you considered taking warfarin or other anticoagulant medication? (sold under brand names of Pradaxa, Eliquis, Xarelto, Savaysa, Jantoven or Coumadin)
- Do you have a reason (bleeding, lifestyle, occupation or frequent falling) to look for a safe alternative to long-term use of a blood thinner that will provide a comparable reduction in risk of stroke?
Success Stories
Thomas Donnelly

L-R: Sunandan Pandya, MD, Medical Director of Echocardiography, Thomas Donnelly, Gunjan Shukla, MD, Clinical Director of Cardiac Electrophysiology, and John Zimmerman, MD, Director of Electrophysiology.
Thomas Donnelly, 67, of Sloatsburg, NY is a Dallas Cowboys fan, a retired Town of Ramapo police officer and a grandfather of four. He is also the 100th Watchman patient at Good Samaritan Hospital, a member of the Westchester Medical Center Health Network.
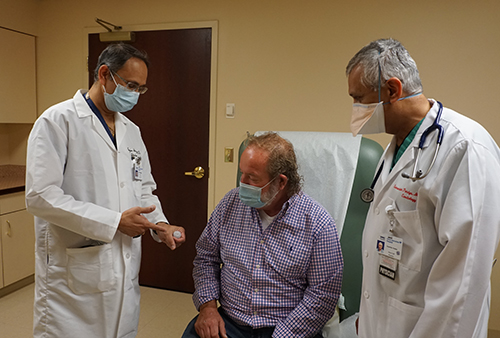 |
| Gunjan Shukla, MD, Clinical Director of Cardiac Electrophysiology (left) and Sunandan Pandya, MD, Medical Director of Echocardiography, show Thomas Donnelly the Watchman device. |
What is Watchman? It is a procedure that implants a device into a part of the heart called the left atrial appendage (LAA) and permanently closes off this part of the heart to keep blood clots from escaping. It is effective in preventing stroke in patients with atrial fibrillation, an abnormal heartbeat, who are unable to tolerate blood thinners.
Mr. Donnelly has been under the care of Cary Hirsh, MD, Co-Director of the Active International Cardiovascular Institute for many years and when he started experiencing a rapid heartbeat, Dr. Hirsch prescribed a blood thinner.
But after a few years, Mr. Donnelly was having trouble tolerating its side effects.
“I was constantly bleeding,” he said. “If my dog would jump on me, and scratch my hand with his paw, I would bleed non-stop. It was a tough medicine to deal with.”
Dr. Hirsch suggested he speak to Gunjan Shukla, MD, Director, Interventional Cardiac Electrophysiology, and John Zimmerman, MD, Director of Electrophysiology, to consider an alternative. The physicians then met with a multi-disciplinary team at Good Samaritan Hospital to verify that Mr. Donnelly was indeed a candidate for the Watchman procedure.
The medical team moved forward to perform the procedure. Sunandan Pandya, MD, Medical Director of Echocardiography, administered a special echocardiogram to guide Dr. Shukla as he implanted the Watchman device.
“Mr. Donnelly’s immediate problem was bleeding. With the Watchman, we were able to close the left atrial appendage of the heart so he doesn’t bleed anymore and at the same time, we prevent him from having a stroke,” said Dr. Shukla.
“My former boss, the Town of Ramapo Police Chief, said ‘You can go anywhere in the world with the insurance we have and we’re a half hour from Manhattan, so why would you go to Suffern, NY?’ I’m happy I did!
“You don’t have to go into New York City when you have a hospital like this right in your backyard,” he added. “Care that I was given here was second to none.
Linda Brancato

.jpg)
Linda Brancato, with her husband, Stan, is happy she finally got the help she needed.
By Deborah Skolnik / Photos by John Halpern
Linda Brancato had a heart rhythm disorder but couldn’t tolerate the medicine that normally treats it. Luckily, a physician at Good Samaritan Hospital offered a minimally invasive treatment.
Having spent 21 years in the fast-paced world of retail sales, Linda Brancato didn’t think anything was amiss when she began to have spells that felt like anxiety attacks. “My heart would race, and I’d get lightheaded and dizzy,” recalls the 67-year-old Monroe resident. “I felt like I had to hold on to someone or something, because I thought I could pass out.”
Life slowed down when Brancato retired, yet her spells only grew longer. A cardiologist performed a range of tests and had her wear a heart monitor. Based on data the device had recorded, she was diagnosed with paroxysmal (or occasional) atrial fibrillation, or AFib, an irregular and often rapid heartbeat.
Blood Thinners Lead to Dangerous Bleeding
During AFib, the heart’s atria (two upper chambers), beat irregularly and out of sync with its two lower chambers. Because of this, blood clots can form in the atria and can then circulate throughout the body. Depending where they end up, these clots can cut off blood supply to organs or cause a stroke or heart attack. “I was disheartened by this news,” Brancato recalls.
She was prescribed a blood thinner to help prevent blood clots. However, the medication’s side effects required an alternative solution to prevent clots without the use of medication.
Answers at Last
She soon learned about a procedure where a device called a Watchman is implanted in the heart to help prevent clots without the use of blood-thinner medication.
She consulted with Gunjan Shukla, MD, an electrophysiologist at Good Samaritan Hospital, a member of WMCHealth. “I left his office with a smile on my face, knowing I was going to get the help I needed.”
Preparing for the Procedure
Two days before her implant, Brancato visited Sunandan Pandya, MD, a cardiologist at Good Samaritan Hospital.
“I performed a transesophageal echocardiogram, also known as a TEE, on Linda,” he says, “to look at the heart in detail.” He took images of her heart and paid particular attention to a pouch within the front of the heart’s left upper chamber, called the left atrial appendage, or LAA, where the majority of blood clots due to AFib form.
The Watchman would be implanted there, sealing it and preventing clot creation. After the TEE, which lasted about 30 minutes, Brancato went home to await her procedure.
The following day, Dr. Shukla performed the Watchman procedure (see sidebar). She stayed overnight in the hospital and was discharged the following day.
Success!
Brancato had a follow-up transesophageal echocardiogram, this time to ensure there were no leaks around the Watchman. Dr. Pandya also checked that the heart’s internal skin, called the endothelium, had grown over the device, covering it as expected. All looked well, and Brancato was cleared to discontinue blood thinners.
While she still manages her AFib with medication, Brancato is not currently symptomatic. Equally important, she no longer needs to worry about the possible side effects of blood thinners. “I have to give a shout-out to everyone I met during this process, from the door greeter at Good Samaritan to the nurses and doctors. I have such gratitude for my nurse coordinator, Suzanne Bartman, for checking in with me and visiting me and guiding me through the process,” she says. “They were all incredible.”
"Do your research on the procedure to familiarize yourself with what is ahead. Make sure you are comfortable with the doctor you choose. — Linda Brancato"